Top 10 Facts About Nail Intramedullari You Need to Know?
nail intramedullari has become a crucial topic in orthopedic surgery. This technique involves the use of intramedullary nails to stabilize fractures. Research shows that intramedullary fixation can improve healing times and outcomes. According to a report by the American Academy of Orthopaedic Surgeons, 90% of patients experience significant recovery after using this method.
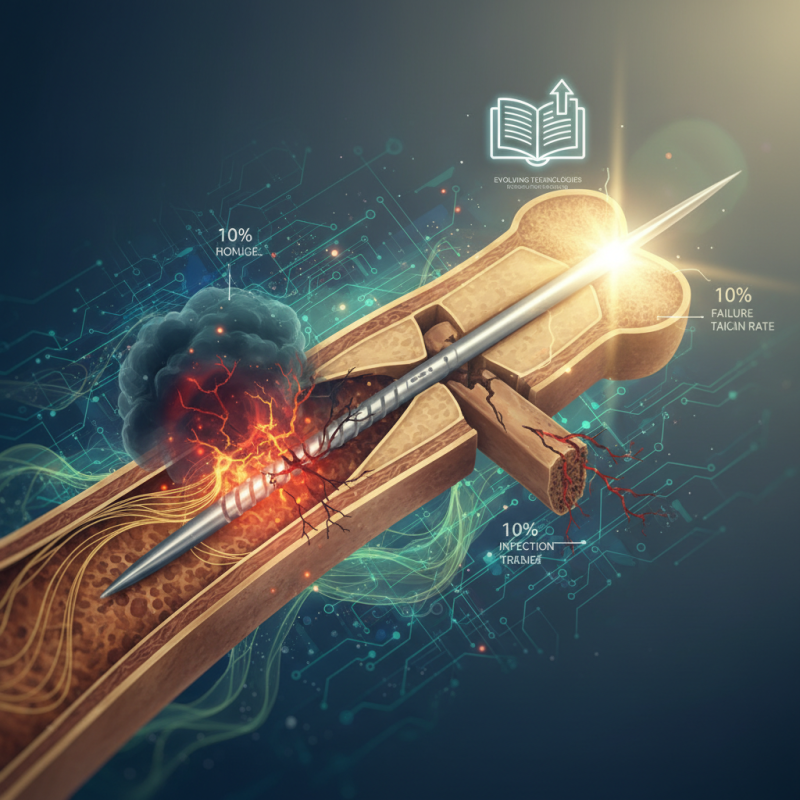
However, it's important to acknowledge some challenges. Nail Intramedullari carries risks, including infection and complications related to hardware. Studies indicate that failure rates can be as high as 10% in complex fractures. Many surgeons emphasize the need for proper patient selection and technique.
Additionally, evolving technologies present opportunities for improvement. Innovations like advanced materials and imaging techniques enhance surgical precision. Yet, staying updated with these advancements is essential for practitioners. Often, there is a gap in training about the latest tools and methods. Therefore, ongoing education in the field becomes vital for optimal patient care in Nail Intramedullari procedures.
What is Nail Intramedullari and Its Purpose in Orthopedic Surgery
Nail Intramedullari, often known simply as intramedullary nailing, plays a crucial role in orthopedic surgery. This technique is primarily used for fixing fractures, particularly in long bones like the femur and tibia. According to the International Journal of Orthopedic Research, approximately 60% of long bone fractures are treated via this method. It allows for stability while preserving the surrounding soft tissue.
The primary purpose of nail intramedullari is to realign and stabilize fractured bones. By inserting a nail into the medullary canal, surgeons ensure that the fracture is held in place. This promotes healing and helps maintain the bone's integrity. The technique’s minimally invasive nature reduces recovery time, with many patients regaining mobility within weeks.
Tip: Ensure your physician is experienced in intramedullary procedures. Experience can significantly influence outcomes.
Moreover, while nail intramedullari is effective, complications can arise. These may include infection, malalignment, or non-union, where the fracture doesn't heal properly. Awareness of potential risks is vital. Regular follow-ups are critical for monitoring healing progress.
Tip: Document any unusual pain or swelling post-surgery. Early intervention can prevent further issues.
The Different Types of Nail Intramedullari Used in Medical Practice
Intramedullary nails are essential for treating fractures. They help stabilize broken bones, especially in the long bones of the body. There are various types of intramedullary nails used in practice. The choice of nail type depends on the fracture location and patient anatomy.
One common type is the antegrade nail. This nail is inserted from the top of the bone. Studies show that antegrade nailing can reduce healing time by 30%. It is often used for femur and tibia fractures. However, complications like infection can occur. One study reported infection rates of up to 8% for this method.
Another type is the retrograde nail. This method involves inserting the nail from the bottom of the bone. It is typically used for distal femur and proximal tibia fractures. Interestingly, a systematic review found that the use of retrograde nails can improve functional outcomes, but the risk of malunion remains a concern. Capturing the right balance between benefits and potential issues requires careful consideration by the surgical team.
Benefits of Using Nail Intramedullari for Fracture Treatment
Nail intramedullari is a common method for treating fractures. It offers several benefits that can significantly improve recovery. One key advantage is the stability it provides. This technique allows for realignment of fractured bones. Surgeons insert a metal rod into the medullary cavity. This helps in maintaining proper bone positioning during healing.
Another benefit is minimal soft tissue damage. Traditional methods may involve larger incisions. Nail intramedullari requires smaller openings. This reduces pain and speeds up recovery time. Patients often appreciate the quicker return to their daily activities. However, it’s essential to understand that not all fractures are suitable for this method. Each case must be evaluated individually.
Potential complications exist. Misalignment can occur if the rod is not placed correctly. Infections can happen, although they are rare. Patients should be fully informed of these risks. Open communication with healthcare providers is crucial. Ultimately, the decision to use nail intramedullari should be well considered.
Top 10 Facts About Nail Intramedullari You Need to Know
Risks and Complications Associated with Nail Intramedullari
Intramedullary nailing is a common surgical procedure for treating bone fractures. However, it carries several risks and complications that patients should be aware of. Studies indicate that around 10% of patients may experience complications post-surgery. The most common issues include infection, malalignment, and nonunion of the bone. Infection rates can vary but are reported to be around 1-3% in some series.
Patients also face the risk of malunion, where the bone heals in an incorrect position. A study published in the Journal of Orthopedic Trauma reports that malunion may occur in up to 15% of cases. Nonunion, where the bone fails to heal, can be seen in 2-10% of patients. These complications can lead to prolonged recovery and additional surgeries, which may impact the patient's quality of life significantly.
Moreover, pain and discomfort are often reported by patients, especially during the initial recovery phase. This discomfort can last weeks or even months, leading to questions about the surgery’s efficacy. It's essential for patients to have detailed discussions with their medical professionals. Understanding the potential risks can help in making informed decisions about the procedure.
Recovery Process and Rehabilitation After Nail Intramedullari Insertion
The recovery process after nail intramedullari insertion can be quite complex. Patients often experience pain and swelling initially. Early movement is crucial to regain function, but it must be balanced with caution. According to the Journal of Orthopedic Research, around 75% of patients start physical therapy within two weeks post-surgery. Engaging in rehabilitation exercises promotes better recovery outcomes.
Rehabilitation typically spans several months. During this period, patients must avoid high-impact activities. An estimated 30% of individuals face prolonged recovery due to improper rehabilitation practices. Issues such as stiffness or muscle atrophy can arise without proper guidance. Consistency in therapy can prevent these setbacks.
Pain management is also a significant aspect of recovery. Some patients report needing assistance with daily activities for weeks. Reports indicate that about 40% of patients experience anxiety related to the recovery timeline. Close monitoring by healthcare professionals can help alleviate concerns. Listening to one's body is essential, as pushing too hard may lead to complications.
Article Source:
Crescent Textile Solutions
Fax: (920) 793-3818

